Supervisor Training Guide
How to Effectively Protect Your Workers from the Dangers of Heat
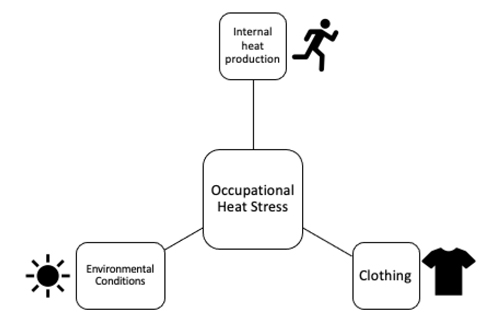
What is Occupational Heat Stress?
Workers can experience heat stress in the workplace through three different ways: 1) environmental heat stress (environmental conditions), 2) heat generated within the body through physical work (internal heat production) and 3) clothing.
Environmental Conditions: Environmental heat through ambient temperature, humidity, solar radiation, other radiant sources of heat (e.g., ovens)
Internal heat production: To meet work demands, workers perform physical work that increases the body’s internal temperature. Heavy exertion and/or prolonged hours of work tend to be associated with greater internal heat production.
Clothing: Many occupations require workers to wear heavy personal protective gear or clothing to protect them from various hazards on the worksite. Wearing encapsulating clothing limits the body's ability to get rid of heat (i.e., limits the body's ability to cool itself) and can result in increased internal body temperature.
What are Heat-related Injuries and Illnesses I should Look for?
As a supervisor, you will be responsive for identifying heat-related injuries and illnesses in your workers. Below is a list of the most common exertional heat-related illnesses and injuries and their corresponding signs and symptoms.
| Exertional Heat Illnesses | Definition | Signs and Symptoms | Treatment |
|---|---|---|---|
| Heat Syncope | A fainting episode due to heat, body temperature is normal | Dizziness, weakness, tunnel vision, decreased or weak pulse, pale or sweaty skin, loss of consciousness | Move worker to shade, sit or lie down worker when symptoms occur, monitor vital signs, elevate legs to promote blood returning to heart, rehydrate |
| Heat-related Cramps | Painful, involuntary muscle spasms (usually occurring in legs) in the heat | Painful, involuntary muscle spasms (usually occurring in legs) in the heat | Adequate fluid and electrolyte replacement, stretching of the muscle, rest |
Heat Exhaustion Illness | Heat-related condition when core temperature between 96.8-105°F | fatigue, nausea, fainting, weakness, vomiting, dizziness, pale, chills, diarrhea, irritability, headache, decreased muscle coordination, | move to shaded area, cool worker (ice bags, ice towels, cooling vests, etc.), remove excess clothing, elevate legs to promote venous return, provide fluids and rehydrate |
| Heat Stroke | A life-threatening medical condition with the following diagnostic criteria: (1) Central Nerve System (CNS) dysfunction and (2) core temperature greater than 105°F (or 40.58 °C). | See Below |
Exertional Heat Stroke (EHS)
This is a medical EMERGENCY!
| Signs | Symptoms |
|---|---|
| Extreme Hyperthermia (greater than 105°F) | Dizziness |
| Altered Consciousness | Headache |
| Disorientation | Nausea |
| Confusion; Look “out of it” | Muscle Cramps |
| Vomiting | Dehydration |
| Staggering | Irritability/Combative |
| Decreased Work Capacity | Muscle Weakness |
| Profuse Sweating | Irrational Behavior |
What do I do if a Worker is Suffering from EHS?
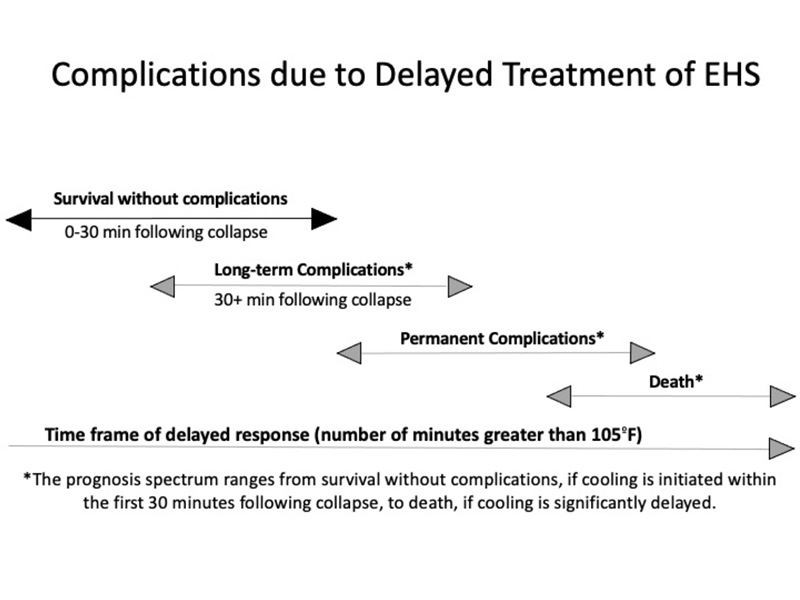
-Call 911 - This is a serious medical emergency!
-Initiate whole body cold water immersion to reduce the workers’ body temperature. Time is CRITICAL.
-Work with EMS to ensure that the worker is cooled appropriately prior to transport to the hospital (cool first, transport second)
-Have an Emergency Action Plan (EAP) in place so you know what to do if something goes wrong! Please got to https://ksi.uconn.edu/emergency-conditions/heat-illnesses/exertional-heatstroke/
heat-stroke-treatment/ for more information on EHS treatment
Other Medical Conditions Caused by Occupational Heat Stress
There are many other medical conditions or injuries that are caused by heat. The dangers of
occupational heat stress are not limited to just heat-related illnesses. The following are
examples of conditions that may be increased under heat stress.
1) Cardiac events
As heat increases cardiovascular strain, it is important to recognize that workers with
cardiovascular risk factors have an increased likelihood of suffering from a serious
cardiac event under heat stress.
2) Kidney Injury
Recent evidence has suggested that dehydration and heat stress are linked to acute
kidney injury, which can increase risk of developing kidney disease.
3) Accidents
Heat can increase risk of accidents as it can negatively affect cognition, decrease
thermal comfort, and alter work site conditions (e.g., fog safety glasses, sweaty hands
cause slippery tools).
Examples of Occupational Factors that Contribute to Heat-related Injury and Illnesses
- Occupational Heat Stress (environment, physical exertion, clothing)
- Limited air movement
- Poor workplace regulations (current heat safety policies and procedures)
- Prolonged work hours
- Worker characteristics
- Lack of heat safety training
- Emphasis on productivity over safety and health
- No environmental monitoring
Examples of Worker Characteristics Associated with Heat Intolerance (Risk Factors)
- Sedentary lifestyle
- Type 1 and Type 2 Diabetes
- Age (i.e., older workers)
- Cardiovascular disease
- Hypertension
- Obesity
- Autonomic Dysfunction (dysfunction of the autonomic nervous system that is in control of automatic, unconscious, and involuntary functions of the body)
- Overzealous (i.e., refusing to take a break)
- Malignant Hyperthermia
- Kidney Disease
- Medications that affect thermoregulation, central nervous system, sodium balance
- Heat Unacclimatized (i.e., workers who are not used to the heat yet)
Prevention
1) Proper Heat Hygiene
Like many other hazards, workers should come to work prepared to perform their job. You should encourage workers to get enough sleep, eat nutritious foods, hydrate, limit alcohol consumption. Coming to work prepared will decrease their risk of experiencing any heat-related injury or illness.
If your workers are experiencing any of the following, they should NOT work and should obtain medical clearance:
- Signs and symptoms of illness or infection
- Fever
- Diaherra
- Vomiting
- Medications that affect thermoregulation, sodium balance or central nervous system function.
2) Hydration
Hydrating before, during and after work can reduce risk of heat-related illness/injury and improve work capacity. As a supervisor, you must provide workers with cool, potable water that they can easily access. They must also have access to a bathroom to further encourage workers to hydrate.
3) Environmental Monitoring and Work to Rest Ratios
Environmental monitoring is the concept of examining the environmental conditions (ambient temperature, humidity, radiant heat) of the worksite. Wet Bulb Globe Temperature is considered the Industrial Standard for environmental monitoring. Based on the environmental conditions, work to rest ratios (how much time a worker should work and rest) should be determined. American College of Governmental Industrial Hygiensist (ACGIH) and National Institute for Occupational Safety and Health (NIOSH) provide work to rest ratios that can be followed.
4) Heat Acclimatization
Heat acclimatization is progressive and repeated exposure to heat that results in beneficial heat adaptations. Examples of these adaptations are increased sweat rates, reduced body temperature, and reduced heart rate. New workers, workers returning from a prolonged work absence (injury or vacation) should undergo a heat acclimatization protocol. This would encompass a 5-7 day protocol where workers are slowly introduced to the heat and the physical work they are expected to perform on the job.
5) Body Cooling
Body cooling acts to reduce internal temperature to alleviate the strain associated with heat stress. As a supervisor, you are encouraged to provide workers with cooling strategies during their rest breaks and during physical work if applicable. Setting up a shaded cooling center with cooling strategies (e.g., cooling vests, forearm immersion) is extremely important to not only protect the health and safety of your workers, but increase productivity.
References:
ACGIH. 2017. “TLVs and BEIs: Threshold Limit Values for Chemical Substances and Physical Agents and Biological Exposure Indices.”
Arbury, Sheila, Matthew Lindsley, and Michael Hodgson. 2016. “A Critical Review of OSHA Heat Enforcement Cases: Lessons Learned.” Journal of Occupational and Environmental Medicine 58(4):359–63. doi: 10.1097/JOM.0000000000000640.
Belval, Luke N., Douglas J. Casa, William M. Adams, George T. Chiampas, Jolie C. Holschen, Yuri Hosokawa, John Jardine, Shawn F. Kane, Michele Labotz, Renée S. Lemieux, Kyle B. McClaine, Nathaniel S. Nye, Francis G. O’Connor, Bryan Prine, Neha P. Raukar, Michael S. Smith, and Rebecca L. Stearns. 2018. “Consensus Statement- Prehospital Care of Exertional Heat Stroke.” Prehospital Emergency Care 22(3):392–97. doi: 10.1080/10903127.2017.1392666.
Bernard, Thomas E., and Candi D. Ashley. 2009. “Short-Term Heat Stress Exposure Limits Based on Wet Bulb Globe Temperature Adjusted for Clothing and Metabolic Rate.” Journal of Occupational and Environmental Hygiene 6(10):632–38. doi: 10.1080/15459620903133642.
Bodin, T., R. García-Trabanino, I. Weiss, E. Jarquín, J. Glaser, K. Jakobsson, R. a. I. Lucas, C. Wesseling, C. Hogstedt, D. H. Wegman, and WE Program Working Group. 2016. “Intervention to Reduce Heat Stress and Improve Efficiency among Sugarcane Workers in El Salvador: Phase 1.” Occupational and Environmental Medicine 73(6):409–16. doi: 10.1136/oemed-2016-103555.
Borg, Matthew A., Jianjun Xiang, Olga Anikeeva, Dino Pisaniello, Alana Hansen, Kerstin Zander, Keith Dear, Malcolm R. Sim, and Peng Bi. 2021. “Occupational Heat Stress and Economic Burden: A Review of Global Evidence.” Environmental Research 195:110781. doi: 10.1016/j.envres.2021.110781.
Brake, D. J., and G. P. Bates. 2003. “Fluid Losses and Hydration Status of Industrial Workers under Thermal Stress Working Extended Shifts.” Occupational and Environmental Medicine 60(2):90–96. doi: 10.1136/oem.60.2.90. Casa, Douglas J., Julie K. DeMartini, Michael F. Bergeron, Dave Csillan, E. Randy Eichner, Rebecca M. Lopez, Michael S. Ferrara, Kevin C. Miller, Francis O’Connor, Michael N. Sawka, and Susan W. Yeargin. 2015. “National Athletic Trainers’ Association Position Statement: Exertional Heat Illnesses.” Journal of Athletic Training 50(9):986–1000. doi: 10.4085/1062-6050-50.9.07.
Casa, Douglas J., Brendon P. McDermott, Elaine C. Lee, Susan W. Yeargin, Lawrence E. Armstrong, and Carl M. Maresh. 2007. “Cold Water Immersion: The Gold Standard for Exertional Heatstroke Treatment.” Exercise and Sport Sciences Reviews 35(3):141–49. doi: 10.1097/jes.0b013e3180a02bec.
Chicas, Roxana, Nezahualcoyotl Xiuhtecutli, Nathan E. Dickman, Madeleine L. Scammell, Kyle Steenland, Vicki S. Hertzberg, and Linda McCauley. 2020. “Cooling Intervention Studies among Outdoor Occupational Groups: A Review of the Literature.” American Journal of Industrial Medicine 63(11):988–1007. doi: 10.1002/ajim.23175.
Flouris, Andreas D., Petros C. Dinas, Leonidas G. Ioannou, Lars Nybo, George Havenith, Glen P. Kenny, and Tord Kjellstrom. 2018. “Workers’ Health and Productivity under Occupational Heat Strain: A Systematic Review and Meta-Analysis.” The Lancet Planetary Health 2(12):e521–31. doi: 10.1016/S2542-5196(18)30237-7.
Jacklitsch B, Williams WJ, Musolin K, Coca A, Kim J-H, Turner. 2016. “Criteria for a Recommended Standard: Occupational Exposure to Heat and Hot Environments - Revised Criteria 2016.” doi: 10.26616/NIOSHPUB2016106.
Kjellstrom, T., D. Briggs, Chris Freyberg, B. Lemke, M. Otto, and O. Hyatt. 2016. “Heat, Human Performance, and Occupational Health: A Key Issue for the Assessment of Global Climate Change Impacts.” doi: 10.1146/annurev-publhealth-032315-021740.