Worker Training Guide
What You Need to Know About the Dangers of Heat
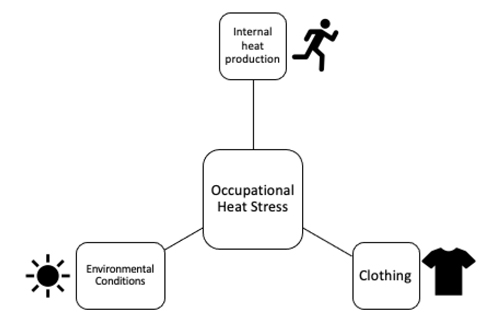
What is Occupational Heat Stress?
You can experience heat stress in the workplace through three different ways: 1) environmental
heat stress (environmental conditions), 2) heat generated within the body through physical work
(internal heat production) and 3) clothing.
Environmental Conditions: Environmental heat through ambient temperature, humidity, solar
radiation, other radiant sources of heat (e.g., ovens)
Internal Heat Production: To meet work demands, you have to perform physical work that may
increase your body’s internal temperature. Heavy exertion and/or prolonged hours of work tend
to be associated with greater internal heat production.
Clothing: Depending on your occupation, you may have to wear heavy personal protective gear
or clothing to protect you from various hazards on the worksite. Wearing encapsulating clothing
limits the body's ability to get rid of heat (i.e., limits the body’s ability to cool itself) and can result
in increased internal body temperature.
What are the Negative Consequences of Heat Stress? Why Should I care?
Heat stress can affect your health, safety, and productivity during work. It's important for you to
be able to identify heat-related illnesses and injuries to protect yourself and other workers.
Below is a list of the most common exertional heat-related illnesses and injuries and their
corresponding signs and symptoms.
| Exertional Heat Illnesses | Definition | Signs and Symptoms | Treatment |
|---|---|---|---|
| Heat Syncope | A fainting episode due to heat, body temperature is normal | Dizziness, weakness, tunnel vision, decreased or weak pulse, pale or sweaty skin, loss of consciousness | Move worker to shade, sit or lie down worker when symptoms occur, monitor vital signs, elevate legs to promote blood returning to heart, rehydrate |
| Heat-related Cramps | Painful, involuntary muscle spasms (usually occurring in legs) in the heat | Painful, involuntary muscle spasms (usually occurring in legs) in the heat | Adequate fluid and electrolyte replacement, stretching of the muscle, rest |
Heat Exhaustion Illness | Heat-related condition when core temperature between 96.8-105°F | fatigue, nausea, fainting, weakness, vomiting, dizziness, pale, chills, diarrhea, irritability, headache, decreased muscle coordination, | move to shaded area, cool worker (ice bags, ice towels, cooling vests, etc.), remove excess clothing, elevate legs to promote venous return, provide fluids and rehydrate |
| Heat Stroke | A life-threatening medical condition with the following diagnostic criteria: (1) Central Nerve System (CNS) dysfunction and (2) core temperature greater than 105°F (or 40.58 °C). | See Below |
Exertional Heat Stroke (EHS)
This is a medical EMERGENCY!
| Signs | Symptoms |
|---|---|
| Extreme Hyperthermia (greater than 105°F) | Dizziness |
| Altered Consciousness | Headache |
| Disorientation | Nausea |
| Confusion; Look “out of it” | Muscle Cramps |
| Vomiting | Dehydration |
| Staggering | Irritability/Combative |
| Decreased Work Capacity | Muscle Weakness |
| Profuse Sweating | Irrational Behavior |
Should we include a section on what to do if someone is suffering from heat stress?
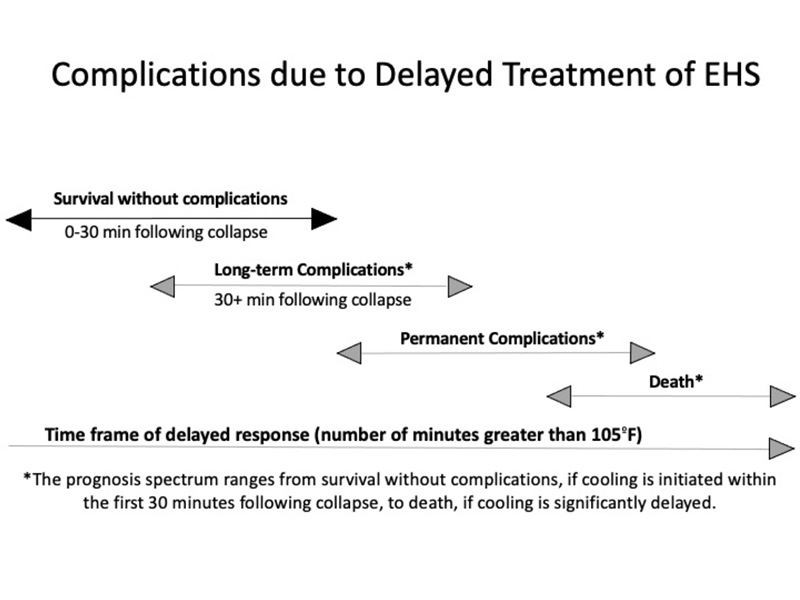
-Call 911 - This is a serious medical emergency! Make sure if you are the one calling, someone is staying with the EHS worker. Make sure your supervisor is immediately notified of the situation to assist or call 911 for you.
-Initiate whole body cold water
immersion to reduce the workers’
body temperature. Time is
CRITICAL.
-Your supervisor should work
with EMS to ensure that the
worker is cooled appropriately prior to transport to the hospital (cool first,
transport second)
Please go to https://ksi.uconn.edu/emergency-conditions/heat-illnesses/exertional-heatstroke/
heat-stroke-treatment/ for more information on EHS treatment
Other Medical Conditions Caused by Occupational Heat Stress
There are many other medical conditions or injuries that are caused by heat. The dangers of
occupational heat stress are not limited to just heat-related illnesses. The following are
examples of conditions that may be increased under heat stress.
1) Cardiac events
As heat increases cardiovascular strain, it is important to recognize that workers with
cardiovascular risk factors have an increased likelihood of suffering from a serious
cardiac event under heat stress.
2) Kidney Injury
Recent evidence has suggested that dehydration and heat stress are linked to acute
kidney injury, which can increase risk of developing kidney disease.
3) Accidents
Heat can increase risk of accidents as it can negatively affect cognition, decrease
thermal comfort, and alter work site conditions (e.g., fog safety glasses, sweaty hands
cause slippery tools).
Examples of Occupational Factors that Contribute to Heat-related Injury and Illnesses
- Occupational Heat Stress (environment, physical exertion, clothing)
- Limited air movement
- Poor workplace regulations (current heat safety policies and procedures)
- Prolonged work hours
- Worker characteristics
- Lack of heat safety training
- Emphasis on productivity over safety and health
- No environmental monitoring
Are YOU at Risk?
There are several factors that may increase your risk of heat-related illness and injury. If you
have any of the following conditions, pay close attention to how you feel while working under
heat stress.
- Sedentary lifestyle
- Type 1 and Type 2 Diabetes
- Age (i.e., older workers)
- Cardiovascular disease
- Hypertension
- Obesity
- Autonomic Dysfunction (dysfunction of the autonomic nervous system that is in control of automatic, unconscious, and involuntary functions of the body)
- Overzealous (i.e., refusing to take a break)
- Malignant Hyperthermia
- Kidney Disease
- Medications that affect thermoregulation, central nervous system, sodium balance
- Heat Unacclimatized (i.e., workers who are not used to the heat yet)
Prevention
1) Proper Heat Hygiene
To avoid the negative consequences of heat stress, you should come to work prepared
to perform your job. You are at a greater risk of heat-related illness if you are:
- Dehydrated
- Sleep deprived
- Fatigued or not recovered
- Experiencing gastrointestinal dysfunction
- Fasted (haven’t eaten)
- Experiencing psychological stress
There are several indications that place you at a high risk of heat-related illness AND will
require that you receive medical clearance prior to engaging in work. You should inform
your supervisor if you are experiencing the following:
- Signs and symptoms of illness or infection
- Fever
- Diarrhea
- Vomiting
- Medications that affect thermoregulation, sodium balance or central nervous system function. ASK YOUR DOCTOR IF YOU ARE NOT SURE.
2) Hydration
Hydration is extremely important to maintain normal body temperatures. You should be
hydrated during rest breaks, before your workshift and after your workshift. Bring your
own water bottle to work if you are able to. To ensure you are hydrated, check your urine
color. If you have light colored urine, it is likely you are hydrated.
3) Body Cooling
Body cooling acts to reduce internal temperature to alleviate the strain associated with
heat stress. You are encouraged to utilize the cooling strategies provided by your
supervisor during their rest breaks and during physical work if applicable. To achieve
optimal benefits from cooling, you should try to perform pre-work cooling and/or post
cooling (for recovery).
References:
ACGIH. 2017. “TLVs and BEIs: Threshold Limit Values for Chemical Substances and
Physical Agents and Biological Exposure Indices.”
Arbury, Sheila, Matthew Lindsley, and Michael Hodgson. 2016. “A Critical Review of
OSHA Heat Enforcement Cases: Lessons Learned.” Journal of Occupational and
Environmental Medicine 58(4):359–63. doi: 10.1097/JOM.0000000000000640.
Belval, Luke N., Douglas J. Casa, William M. Adams, George T. Chiampas, Jolie C.
Holschen, Yuri Hosokawa, John Jardine, Shawn F. Kane, Michele Labotz, Renée S.
Lemieux, Kyle B. McClaine, Nathaniel S. Nye, Francis G. O’Connor, Bryan Prine, Neha
P. Raukar, Michael S. Smith, and Rebecca L. Stearns. 2018. “Consensus Statement-
Prehospital Care of Exertional Heat Stroke.” Prehospital Emergency Care 22(3):392–
97. doi: 10.1080/10903127.2017.1392666.
Bernard, Thomas E., and Candi D. Ashley. 2009. “Short-Term Heat Stress Exposure
Limits Based on Wet Bulb Globe Temperature Adjusted for Clothing and Metabolic
Rate.” Journal of Occupational and Environmental Hygiene 6(10):632–38. doi:
10.1080/15459620903133642.
Bodin, T., R. García-Trabanino, I. Weiss, E. Jarquín, J. Glaser, K. Jakobsson, R. a. I.
Lucas, C. Wesseling, C. Hogstedt, D. H. Wegman, and WE Program Working Group.
2016. “Intervention to Reduce Heat Stress and Improve Efficiency among Sugarcane
Workers in El Salvador: Phase 1.” Occupational and Environmental Medicine
73(6):409–16. doi: 10.1136/oemed-2016-103555.
Borg, Matthew A., Jianjun Xiang, Olga Anikeeva, Dino Pisaniello, Alana Hansen, Kerstin
Zander, Keith Dear, Malcolm R. Sim, and Peng Bi. 2021. “Occupational Heat Stress and
Economic Burden: A Review of Global Evidence.” Environmental Research
195:110781. doi: 10.1016/j.envres.2021.110781.
Brake, D. J., and G. P. Bates. 2003. “Fluid Losses and Hydration Status of Industrial
Workers under Thermal Stress Working Extended Shifts.” Occupational and
Environmental Medicine 60(2):90–96. doi: 10.1136/oem.60.2.90.
Casa, Douglas J., Julie K. DeMartini, Michael F. Bergeron, Dave Csillan, E. Randy
Eichner, Rebecca M. Lopez, Michael S. Ferrara, Kevin C. Miller, Francis O’Connor,
Michael N. Sawka, and Susan W. Yeargin. 2015. “National Athletic Trainers’
Association Position Statement: Exertional Heat Illnesses.” Journal of Athletic Training
50(9):986–1000. doi: 10.4085/1062-6050-50.9.07.
Casa, Douglas J., Brendon P. McDermott, Elaine C. Lee, Susan W. Yeargin, Lawrence
E. Armstrong, and Carl M. Maresh. 2007. “Cold Water Immersion: The Gold Standard
for Exertional Heatstroke Treatment.” Exercise and Sport Sciences Reviews 35(3):141–
49. doi: 10.1097/jes.0b013e3180a02bec.
Chicas, Roxana, Nezahualcoyotl Xiuhtecutli, Nathan E. Dickman, Madeleine L.
Scammell, Kyle Steenland, Vicki S. Hertzberg, and Linda McCauley. 2020. “Cooling
Intervention Studies among Outdoor Occupational Groups: A Review of the Literature.”
American Journal of Industrial Medicine 63(11):988–1007. doi: 10.1002/ajim.23175.
Flouris, Andreas D., Petros C. Dinas, Leonidas G. Ioannou, Lars Nybo, George
Havenith, Glen P. Kenny, and Tord Kjellstrom. 2018. “Workers’ Health and Productivity
under Occupational Heat Strain: A Systematic Review and Meta-Analysis.” The Lancet
Planetary Health 2(12):e521–31. doi: 10.1016/S2542-5196(18)30237-7.
Jacklitsch B, Williams WJ, Musolin K, Coca A, Kim J-H, Turner. 2016. “Criteria for a
Recommended Standard: Occupational Exposure to Heat and Hot Environments -
Revised Criteria 2016.” doi: 10.26616/NIOSHPUB2016106.
Kjellstrom, T., D. Briggs, Chris Freyberg, B. Lemke, M. Otto, and O. Hyatt. 2016. “Heat,
Human Performance, and Occupational Health: A Key Issue for the Assessment of
Global Climate Change Impacts.” doi: 10.1146/annurev-publhealth-032315-021740.